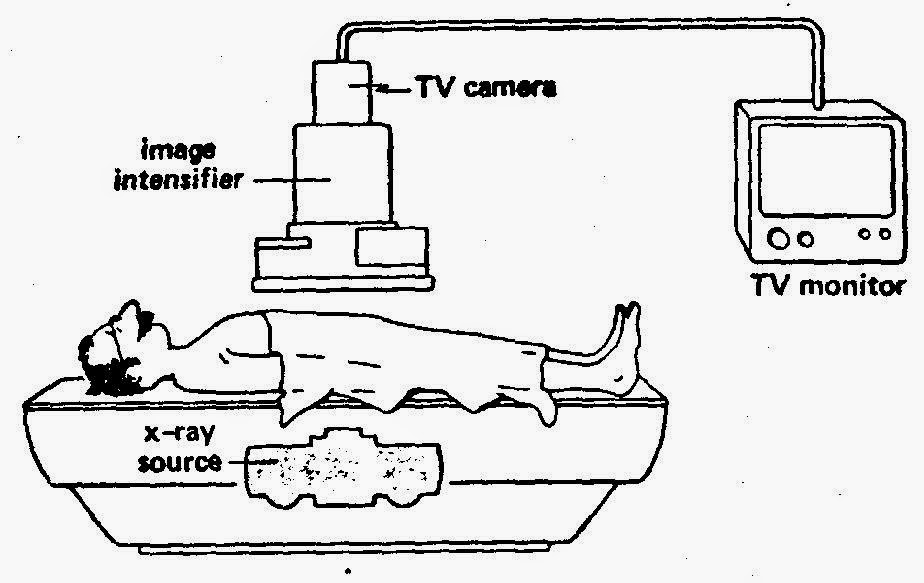
Fluoroscopes have come a long way over the years and are still used today in areas such as orthopedic surgery, gastrointestinal investigations, and angiography but, of course, the dose of x-rays a patient receives is minimized and closely monitored. Have a look at this machine from Siemen’s. “Beam me up Scotty!”.
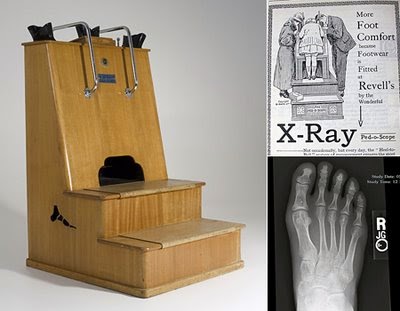
Fluoroscopes have come a long way over the years and are still used today in areas such as orthopedic surgery, gastrointestinal investigations, and angiography but, of course, the dose of x-rays a patient receives is minimized and closely monitored. Have a look at this machine from Siemen’s. “Beam me up Scotty!”.  Due to the enormous supply of portable x-ray machines at the time following the end of the war, Dr Jacob Lowe introduced the idea of using a modified portable x-ray machine in the shoe retail industry. Voila, fried feet fricassee for the next 50 years!
Due to the enormous supply of portable x-ray machines at the time following the end of the war, Dr Jacob Lowe introduced the idea of using a modified portable x-ray machine in the shoe retail industry. Voila, fried feet fricassee for the next 50 years!Now If were to be interested in using a fluoroscope to look at my feet I may be inclined to use a suit like this gentleman below is sporting…
 |
| WW I x-ray protection suit |
Now for the fun part, using Fluoroscope in a sentence by the end of the day:
Serious: Bob, did you know that the foot-o-scope was a modified fluoroscope used to view ones feet when fitting new shoes which delivered on average 13 Roentgens for every 20 second exposure?
Less serious: I heard grampa grumbling he can never find shoes that fit right anymore since they banned fluoroscopes in shoe stores. What is a fluoroscope mommy?
Listen to High Heels to decompress and I’ll see you in the blogosphere.
Pascal Tyrrell