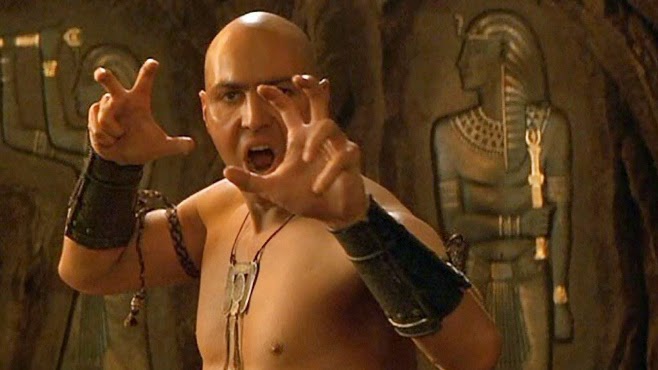
Who hasn’t thought of having Magneto’s powers? No? Maybe you should watch this Magneto trailer for a refresher.
Ok, now that we all want to be Magneto (secretly at least) what is it that is so appealing with having the power of magnetism? Bill Nye the Science Guy explains it very well in this clip. Have a gander.
In a nutshell, magnetism is a physical phenomena that consists of a field of energy created by “magnets” that attracts or repels other objects. Magnets come in two major flavors: permanent magnets made of materials (such as iron) and electromagnets – the strongest and most widely used in medical imaging.
Interestingly, it is the sum of the magnetic fields of individual electrons that is responsible for all the fun (see quantum mechanics). In the case of electromagnetism the electric current in a wire produces a magnetic field in the same direction of the current. In the case of a permanent magnet it is the magnetic fields of the naturally occurring electrically charged particles of the atoms that make up the material (iron for example) that are responsible. However, for there to exist a force strong enough to attract or repel another object all of its magnetic ions must have their magnetic fields aligned and contributing to the net magnetization. This is how you can magnetize a needle when stroking it in a uniform directional way with a permanent magnet.
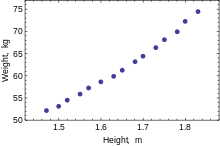
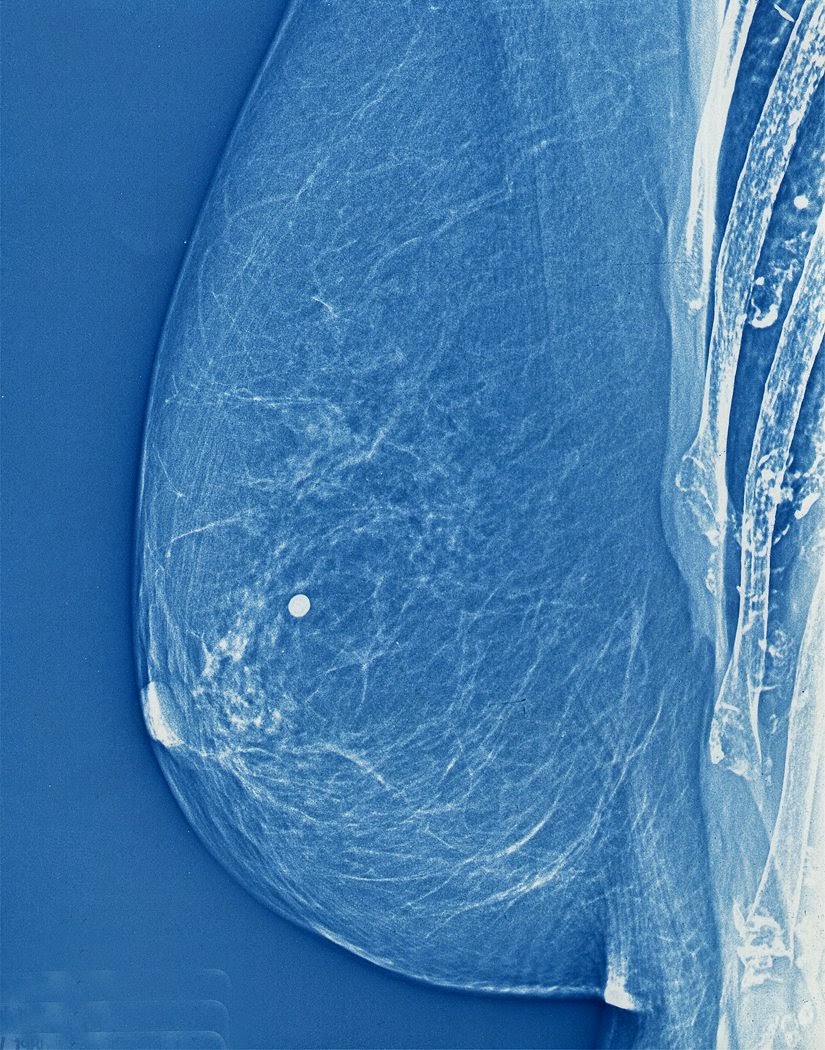
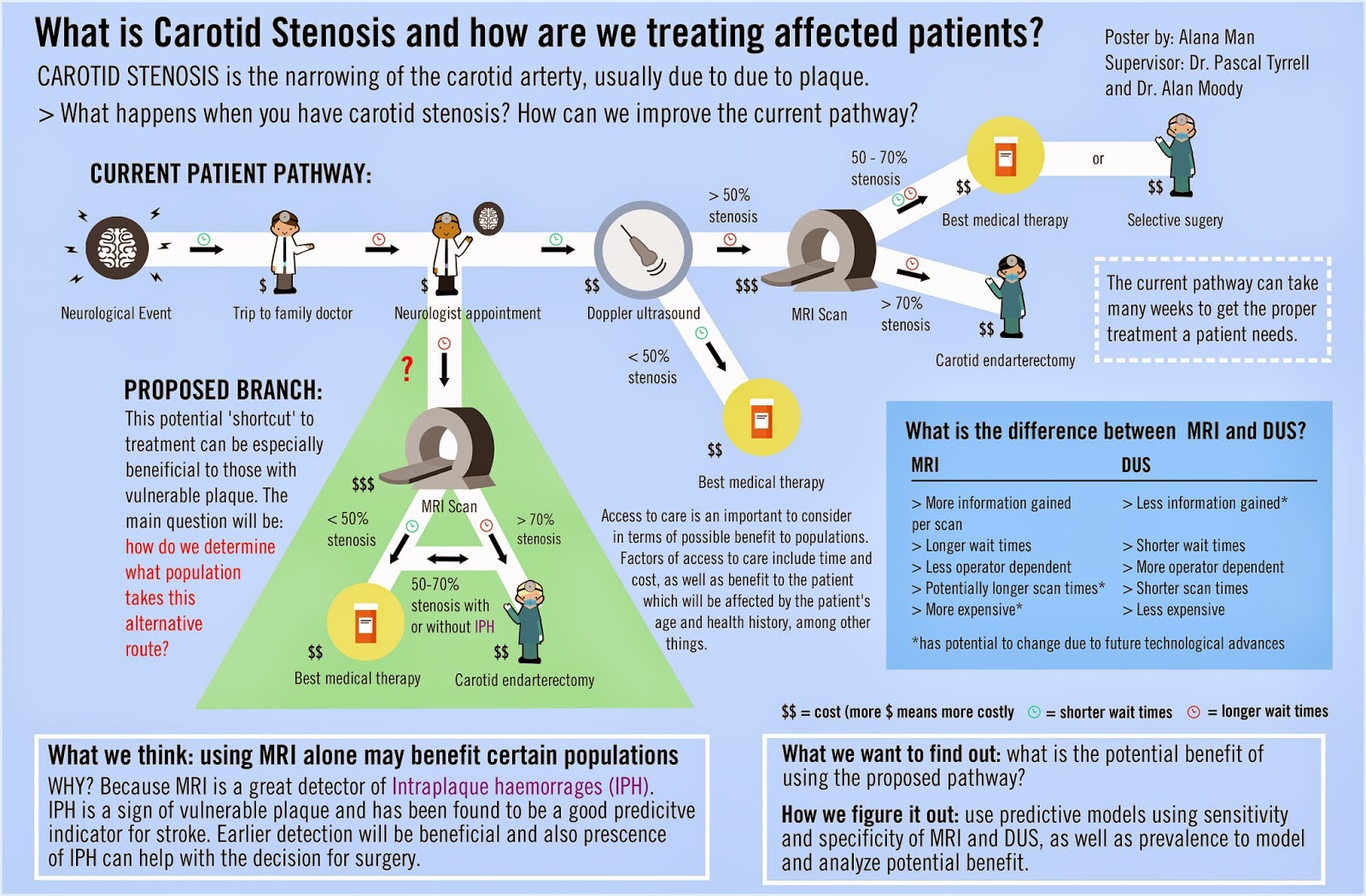
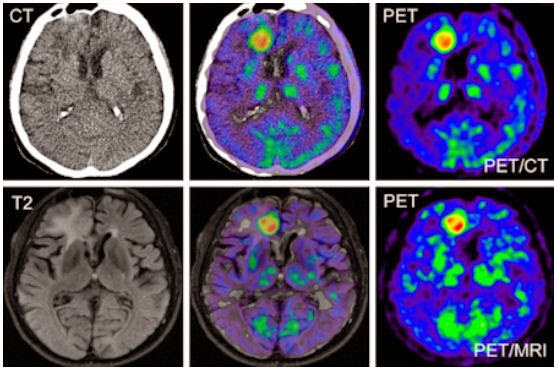
.jpg) Magnetism is to MRI what radiation is to X-rays. The strength of magnets is measured in gauss and Tesla units. There are 10,000 gauss to a Tesla and the earth’s magnetic field is one half of a gauss. Today most clinical MRIs use superconducting magnets whose strength range up to 4 Tesla! Experimental MRIs can run up to 10 Tesla. Now that is more Magneto’s speed.
Magnetism is to MRI what radiation is to X-rays. The strength of magnets is measured in gauss and Tesla units. There are 10,000 gauss to a Tesla and the earth’s magnetic field is one half of a gauss. Today most clinical MRIs use superconducting magnets whose strength range up to 4 Tesla! Experimental MRIs can run up to 10 Tesla. Now that is more Magneto’s speed.
The powerful magnets allow for better spacial resolution allowing for better sensitivity of the image. However, all this magnetic strength comes at a cost: the production of chemical shift artifacts – ghosts of things that are not really there. This is why we have radiologists to make sense of it all.
OK. Now you are asking what the heck. Magneto in the X-Men movie was able to rip out the iron from a human so why doesn’t an MRI? Great question. Iron found in the human body is mostly found as ferritin (a type of iron oxide) and is NOT magnetic. The iron in hemoglobin is also NOT magnetic. Bummer. So how does Magneto do it? Well either the movie is not scientifically correct (now that would be a shocker) or possibly he could be drawing on magnetite (another iron oxide) that is magnetic and has been found in trace amounts in the blood and brain. It is so little though that it does not cause any concern for MRI. Oh well, so much for Magneto…
Now for the fun part (see the rules here), using magnet in a sentence by the end of the day:
Serious: Hey Bob, did you know that early MRI machines used permanent magnets?
Less serious: Went for my MRI today. Told them I was worried the MRI would rip all the iron out of my blood like in X-Men. They didn’t even know who Magneto was. Whaaaat?!!
OK, listen to Magnetic by Traphik to decompress and I’ll see you in the blogosphere…
Pascal Tyrrell