 |
| Stella Song ROP Summer 2016 |
I am Stella Bing Xin Song, currently a second year student studying pharmacology and psychology at University of Toronto. I was fortunate to be a part of the 2016 Research Opportunity Program (ROP) supervised by Dr. Pascal Tyrrell in the Department of Medical Imaging at University of Toronto.
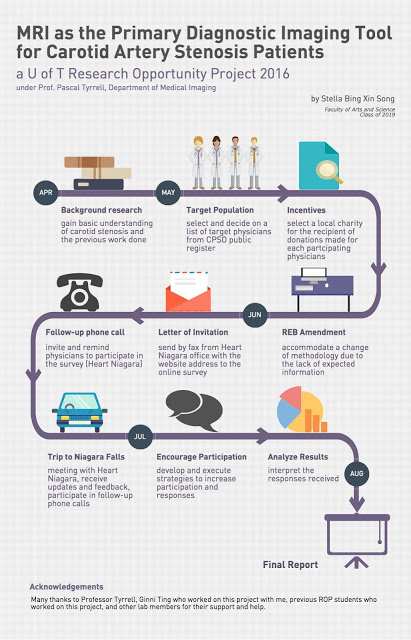
 My ROP project focused on evaluating the feasibility of using MRI as the primary imaging modality for carotid artery stenosis diagnosis and assessment (not sure what we are talking about? See previous posts here and here). Along with Ginni Ting, a student volunteer in Dr. Tyrrell’s lab, we surveyed physicians in the Niagara region of Ontario to learn about their perspectives on this proposal. Our community partner in this research was Heart Niagara – a fantastic local organization that has been guiding advances in cardiac health education and services since 1977.
My ROP project focused on evaluating the feasibility of using MRI as the primary imaging modality for carotid artery stenosis diagnosis and assessment (not sure what we are talking about? See previous posts here and here). Along with Ginni Ting, a student volunteer in Dr. Tyrrell’s lab, we surveyed physicians in the Niagara region of Ontario to learn about their perspectives on this proposal. Our community partner in this research was Heart Niagara – a fantastic local organization that has been guiding advances in cardiac health education and services since 1977. Unfortunately, the response rate for this online survey was very low. Reasons given for the reluctance to participate were that physicians were on a tight schedule and were busy with their patients. Feedback from participants was that the online survey seemed long. Nevertheless, from the responses received, we were able to learn more about physicians’ perspectives of using MRI for carotid artery stenosis diagnosis and assessment.
Unfortunately, the response rate for this online survey was very low. Reasons given for the reluctance to participate were that physicians were on a tight schedule and were busy with their patients. Feedback from participants was that the online survey seemed long. Nevertheless, from the responses received, we were able to learn more about physicians’ perspectives of using MRI for carotid artery stenosis diagnosis and assessment.In the end, it was an exciting and valuable experience to plan out and execute this research project. Most importantly, I had the pleasure to join Dr. Tyrrell’s lab and meet his team. I am grateful for all the help and support which I have received throughout my time at the lab. I look forward to continuing to work as a member of Dr. Tyrrell’s lab.
Stella Bing