OK who hasn’t made rock candy as a kid? No? Give it a try. Maybe you have a little brother or sister you can impress. All you need is a super saturated solution of sugar, a surface for crystal nucleation (string), and lots of time…
OK who hasn’t made rock candy as a kid? No? Give it a try. Maybe you have a little brother or sister you can impress. All you need is a super saturated solution of sugar, a surface for crystal nucleation (string), and lots of time…
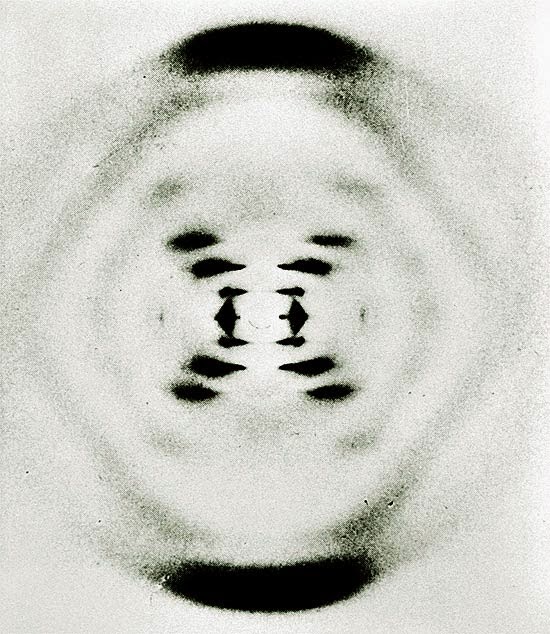
Now what if you were to apply this technique to obtain crystals of DNA? I don’t suggest that you eat it as a treat but you could possibly try X-ray crystallography.
The challenge is that DNA, unlike proteins, is an exceedingly large molecule which does not lend itself to crystallisation. The result is a highly viscous suspension of spiderweb-like filaments. However, it is this very suspension that the DNA molecules were deduced to be neatly aligned alongside one another by studying the X-ray diffraction patterns. This initial challenge was successfully overcome by Rosalind Franklin. Her hard work then laid the ground work for Watson and Crick to piece together the puzzle of DNA structure (winning the 1962 Nobel Prize along with Wilkins).
Now the x-ray crystallography imaging technique is no pic-nic! It was first described by the Australian father-and-son duo William Henry Bragg and William Lawrence Bragg. Essentially x-rays are projected onto a crystalline solid and when analyzing the diffraction patterns it is possible to determine how its molecular atoms are positioned in relation to one another. This is due to x-rays having very short wave-lengths (see x-rays in the blog) and the mathematical analysis of predictable diffraction from the three dimensional structure of the crystal. It was Lawrence Bragg who developed the equation to describe this diffraction and is now known as Bragg’s Law. He and his father won the Nobel Prize for this work in 1915.
I used to listen to New Order back in the day and they are still singing (and dancing?) with a more recent release of Crystal by New Order. So, listen to the song while making rock candy and maybe you too will come up with a brilliant idea worthy of a Nobel Prize by the time the crystals are big enough to eat.
Now if you remember the rules:
1- I introduce and discuss a word.
2- You have to use the word in a sentence by the end of the day. No need to use it in the correct context – actually out of context is more fun and elicits a more entertaining response!
Today, we have to use “Bragg” in a sentence. Here are two examples to help you along:
The Adventures of Alana the Newbie Researcher
 |
| Timeline of my ROP experience |
Helena Lan: Summer 2014 ROP
 |
| Helena Lan Summer 2014 ROP |
What is research like? If you had asked me this
question several months ago, I would have answered, “You wear a lab coat and
goggles while mixing chemicals or observing organisms. Hopefully something
interesting will happen, so that you get to publish your findings!” Well, after
participating in the Research Opportunity Program (ROP) at the University of
Toronto, I discovered that medical imaging research is more than just
pipetting, and is all the more exciting!
way. Also, I’m very grateful to Dr. Alan Moody for including us in his research program at Sunnybrook, as well as other members of the VBIRG group who gave us the chance to
participate in various activities. My summer would not have been this fun and meaningful without all of your help!
Helena Lan
MiWord of the Day is… Supernova!
So, what does medical imaging have to do with a Supernova? Well in the B-movie – Supernova a deep space medical ship responds to a distress signal from a nearby mining planet and gets too close to a Red Supergiant ready to go Supernova. Is your geek alert tingling?
Well, believe it or not Supernovas are explosions of giant stars. Nuclear fusion produces iron in the cores of these stars. Such dense matter at the core creates a tendency for the star to collapse on itself due to gravitational pull. This is kept in check by the massive amounts of energy the star is constantly releasing. But what happens when the star starts to run out of fuel? Yup, you guessed it. It collapses on itself and implodes. As the star rushes inwards, protons and electrons combine to produce neutrons that in turn collide with the core and produce a crazy big explosion. This sudden release of energy is accompanied by the production of x-rays. Yes, I am serious. What is left behind of the exploded star is either a neutron star or a black hole depending on the mass of the remains.
So, a supernova is essentially a giant x-ray machine? Maybe not. However, by studying these cosmic x-rays astronomers are able to help describe the structure of the universe (not Castle Greyskull). Cool.
Question for you: should we be concerned with being exposed to cosmic x-rays? No. Cosmic x-rays are pretty much completely filtered out by our atmosphere by the time they get to the surface. So, how do astronomers get readings? Good question. By placing their recording instruments on satellites and spacecraft, of course!

Now on to using supernova in a sentence today:
Serious example – So did you catch the last supernova in our galaxy? Happened about 400 years ago. No? The next one should be soon as it is overdue by about 300 years.
Less serious – Growing up I always loved the Chevy Nova SS. Especially when it was customized. It surely was a super Nova…
Enjoy Ray LaMontagne – Supernova to recover from today’s post and I’ll see you in the blogosphere.
Pascal Tyrrell
MiWord of the Day Is… Pentimenti!
What!!? Do you find it on pizza or in the middle of green olives? Well actually, it is a word of Italian origin and describes minor changes in a painting during its composition. So, similar to erasing some of your hand writing and then writing over it again with the corrected text. I guess for you younger folk it would be like pressing back-space and then re-typing! The difference of course is that there would NOT be any pentimenti as there would no trace of your previous attempt…
So what does this have to do with medical imaging? In our last Mi word of the day we talked about x-rays. Now, today we take x-rays and our ability to peer inside the human body for granted. So what else can we see with x-rays? Believe it or not x-rays can also help to reveal how a painting evolved from first brush strokes to finished product. X-ray analysis can help to describe the paint composition to the different layers that may exist in the painting.
Consider, for example, “Patch of Grass” by Van Gogh seen above. It was discovered by x-ray analysis that this 1887 painting completely concealed a portrait of a woman that Van Gogh had painted over. He often did this to save money on canvases (maybe to buy Absinthe – how naughty!). In this case, in addition to Van Gogh’s pentimenti is his habit of painting over previous works. All of this adds to a type of “fingerprint” that art appraisers use to identify works of art from forgeries… Cool.
Today, we have to use “pentimenti” in a sentence (see rules here). Here are two examples to help you along:
Serious: I wonder how Van Gogh’s pentimenti differs from that of Rembrandt. Maybe I should ask the Musee du Louvre’s curator for some insight.
See you in the blogosphere,
Pascal Tyrrell
MiWord of the Day Is… Roentgen!
Welcome to the first Medical imaging Word of the Day! Here is how it works:
1- I introduce and discuss a word.
2- You have to use the word in a sentence by the end of the day. No need to use it in the correct context – actually out of context is more fun and elicits a more entertaining response!
OK, here we go. The word of the day is Roentgen – typically pronounced “Rent-gun”.
Wilhelm Roentgen was a physicist from northern Germany who in 1895 was the first to detect the now famous x-ray. Interestingly, he was not the first to produce them. The x-ray is part of the electromagnetic spectrum that contains shorter wavelengths (0.01 to 10 nm) than visible light (390-700 nm). We will talk about this in another post as today it is about Roentgen.
- Following his discovery the “Roentgen unit” was described and used to measure x-ray exposure (one R is 2.58×10−4 C/kg). About 500 R over 5 hours is considered a lethal dose for humans.
- Roentgen was the first scientist to receive the Nobel prize in physics in 1901. He refused to patent his discovery and gave the entire prize money to his university. Wow, what a guy!
- He died of colon cancer in 1923.
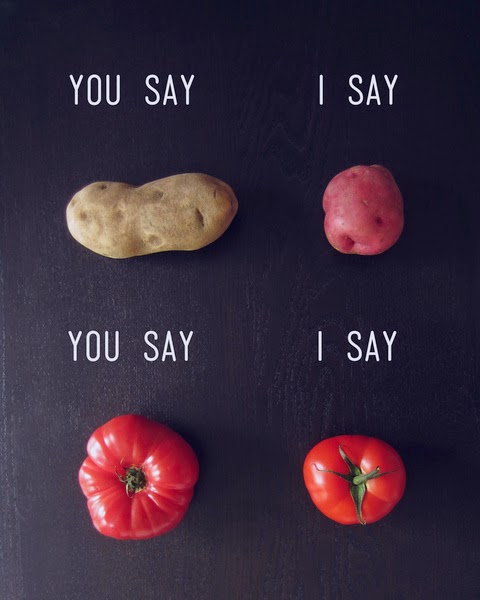
You like potato and I like potahto… Let’s Call the Whole Thing Off!
We have been talking about agreement lately (not sure what I am talking about? See the start of the series here) and we covered many terms that seem similar. Help!
Before you call the whole thing off and start dancing on roller skates like Fred Astaire and Ginger Roberts did in Shall We Dance, let’s clarify a little the difference between agreement and reliability.
When assessing agreement in medical research, we are often interested in one of three things:
1- comparing methods – à la Bland and Altman style.
2- validating an assay or analytical method.
3- assessing bioequivalence.
Agreement represents the degree of closeness between readings. We get that. Now reliability on the other hand actually assesses the degree of differentiation between subjects – so one’s ability to tell subjects apart from within a population. Yes, I realize this is a subtlety just as Ella Fitzgerald and Louis Armstrong sing about in the original Let’s Call the Whole Thing Off.
Now, often when assessing agreement one will use an unscaled index (ie a continuous measure for which you calculate the Mean Squared Deviation, Repeatability Standard Deviation, Reproducibility Standard Deviation, or the Bland and Altman Limits of Agreement) whereas when assessing reliability one often uses a scaled index (ie a measure for which you can calculate the Intraclass Correlation Coefficient or Concordance Correlation Coefficient). This is because a scaled index mostly depends on between-subject variability and, therefore, allows for the differentiation of subjects from a population.
Ok – clear as mud. Here are some very basic guidelines:
1- Use descriptive stats to start with.
2- Follow it up with an unscaled index measure like the MSD or LOI which deal with absolute values (like the difference).
3- Finish up with a scaled index measure that will yield a standardized value between -1 and +1 (like the ICC or CCC).
Potato, Potahtoe. Whatever.
Entertain yourself with this humorous clib from the Secret Policeman’s Ball and I’ll…
See you in the blogosphere!
Pascal Tyrrell
Michener Institute Series: Princess Margaret Hospital, Toronto, Ontario
As first year Radiation Thearpy students here a The Michener Institute, we are currently in our 4th week of clinical placements! As promised, here’s a little update about the experiences Jennifer and Ori are going through at Princess Margaret Hospital.
Jennifer: I’ve been placed in Unit 10 which specializes in treating patients with Genitourinary, Gynae and Lower Gastrointestinal cancer.
Ori: I’m on Unit 14 and we treat breast cancer and palliative cancers.
We are proud to say that we are enjoying our experience here. Our duty as students in training is to follow the radiation therapist and learn what they do. The job of a therapist is to treat cancer using a machine called Linear Accelerator (Linac) to deliver ionizing radiation. Patients will typically come once a day for the next couple of weeks, so we see the same patients every day and therefore really get to know our patients well. There is a fair amount of patient interaction, which is one of our favorite parts of the job. Along with patient interactions, we also get to use the equipment, which mainly includes operating the Linac machine (the machine that delivers the radiation) and taking X-rays or CT scans to make sure the patient is in the right position. Every day is a new experience and we are constantly learning new skills. We get a better insight of the patient’s perspective during the entire span of their radiation treatment. For example most patients in unit 10 are required to have a full bladder and empty rectum. Having to hold their pee can be quite difficult for some patients, especially when there are delays, which pushes Unit 10 to be a very fast paced environment. Overall our first 4 weeks of clinical has been an exceptionally valuable experience and we’re looking forward to our next 4 weeks!
Michener Institute Series: Clinical Placement Site – Kingston Ontario
completing my placement in Kingston General Hospital (KGH) here at Kingston, Ontario. Kingston is a nice beautiful town located at the north side of the entrance of outflow of St Lawrence River from Lake Ontario; it was the first capital of Canada when Canada was still a province of British colony.
practice is eye-opening and a bit hectic; because each patient is unique and no knowledge from books can prepare you how to interact with all patients. It is interesting to learn from the therapists, the way they educate patients on their first day of treatment, the type of approach to each patient base on the assessment they do during the conversation with them. It’s amazing how much compassion the therapists have for patients and how much they care for them.
The Key to Research: (Key)Words
Yes, you are not the only one, many people use Google to further explore some of the things they have come across throughout daily encounters. For each instance google is used, whether it be for a song or for neuroscience research and analysis, one thing remains in common: keywords.
Keywords are essential when searching for various types of information, and the options appearing on any search engine are dependent on the keywords given. How does one establish appropriate keywords for a search engine entry?
Faith Balshin